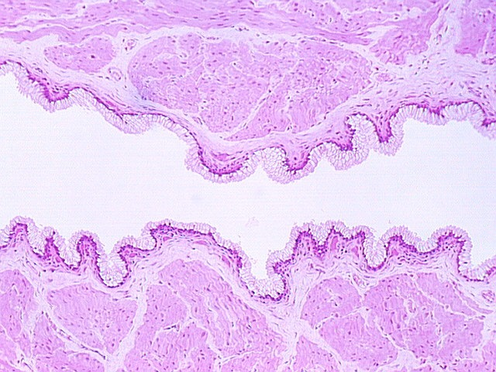
The uterus is a muscular sac, lined with epithelium that undergoes cyclic changes. The wall is made up of thick smooth muscle, organized in interlacing bundles that run randomly. It is called the myometrium In the above photograph, the uterine glands (a part of the endometrium) are seen as straight tubular glands leading to a main lumen. This is diagnostic of the early stage of the cycle or the Proliferative phase. What hormone is secreted by the follicle during this early stage of the cycle?
As stated above, the uterine lining consists of glands that are called "endometrium" As the ovary and oviduct are undergoing changes with the cycle, the uterine lining is being prepared to receive an embryo. The normal human menstral cycle is divided into three phases by the hormonal events and changes in the uterine lining. The first phase is called the Proliferative phase. This coincides with the rise in estrogens early in the cycle and is distinguished in the uterus by lengthening endometrial glands.
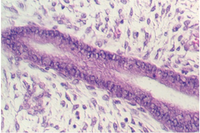
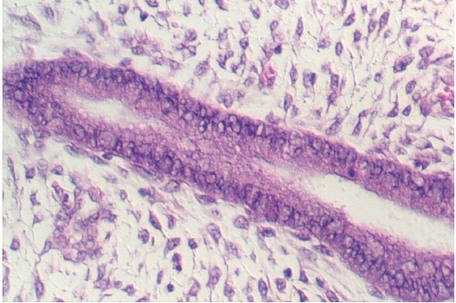
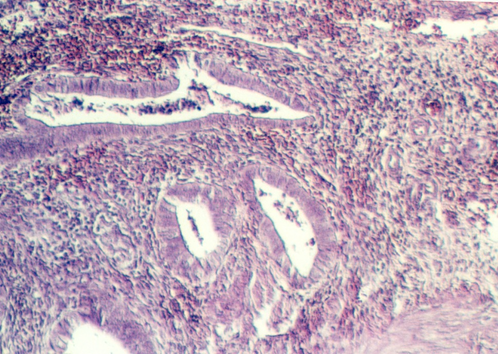
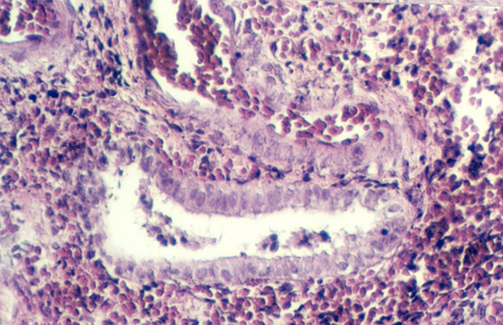
Slide 86 shows a uterus in the proliferative phase. The endometrium is illustrated in the photograph below. Note that the cells are low columnar to high columnar. The glands are relatively straight with a narrow lumina. Outside the glands is the highly cellular lamina propria. The following photos illustrate the proliferative phase with higher magnifications.

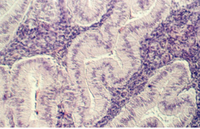
After ovulation, the uterine lining becomes more tortuous. The lining is now under the control of progesterone. This steroid hormone stimulates the lining to secrete material that may help nourish both sperm and a potential pregnancy. The glands expand and the lumina are wide and contain products of secretion. The glandular epithelium may be characterized by a droplet of secretory material under the nucleus (near the base) about 2 days after ovulation (day 16). Then, the secretory products move more towards the lumen. Slide 87 shows the Secretory phase of the uterine lining. Note the sections showing coiled or tortuous glands and the dense lamina propria.

Which cells secrete the progesterone during the uterine secretory phase?
If a pregnancy does not occur, the uterine lining breaks down about 2 weeks after ovulation. Spiral arteries supplying the outer region of the uterine lining constrict and deprive the region of oxygenated blood. The cells lose fluid and cease to function. The stroma is invaded by leukocytes. Necrosis continues and the uterine lining is shed. This is the Menstral phase of the uterine lining. After the third or fourth day, all of the lining is shed except basal regions containing glands that can regenerate during the proliferative phase of the subsequent cycle. The following photograph illustrates the endometrium in the menstral phase. Note the few remaining glands. This region is called the BASALIS, whereas the region that is lost during menstruation is called the FUNCTIONALIS. The glands in the functionalis are the ones that become long during proliferative phase and tortuous during the secretory phase. Note the extravasated blood in the stroma of the endometrium.
The following photograph illustrates uterine myometrium showing the smooth muscle layers running in interweaving bundles.
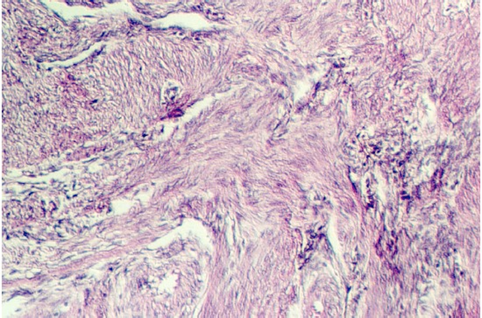
Myometrium is responsive to a hormone that is particularly high during labor. What hormone is this and where is it produced and stored?
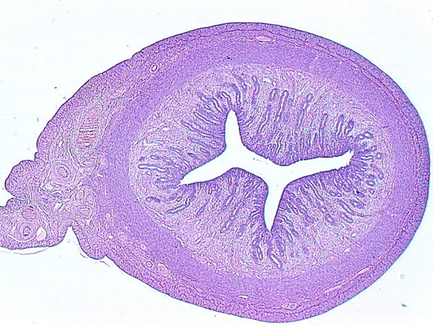
The uterus communicates with the outside world via a short canal called the cervix. The following photograph shows the uterus in the proliferative stage. The glands continue into the cervix in the left side of the photo.
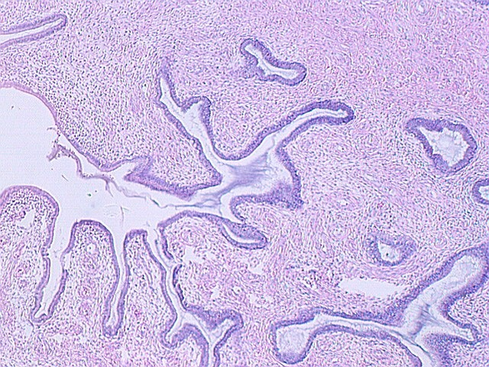
The cervix continues and joins with the vagina. The cervix is lined by simple high columnar epithelium which consists of mucous cells. These are shown in the following views. In the lowest magnification, one can see bundles of smooth muscle in the wall (see below)

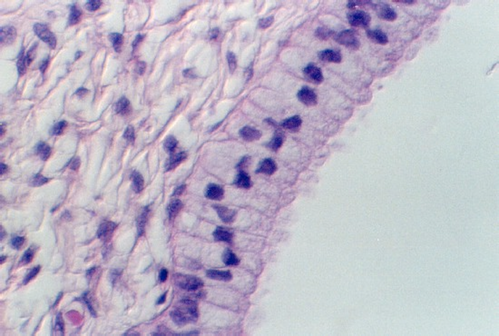
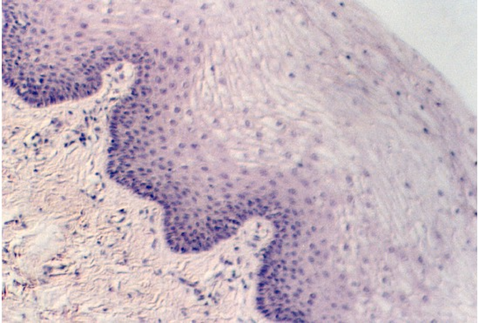
Moving toward the vagina, one can see the abrupt transition between the cervical glands and the stratified squamous epithelium of the vagina. The region showing the vaginal and cervical areas juxtaposed is seen in the following photo.


A low magnification view of the vagina is shown in this photograph. The epithelium is stratified squamous. Underneath the epithelium is a lamina propria. Note that there is no muscularis mucosa. You will use this feature to distinguish the vagina from the esophagus. Another difference is the fact that the vagina has some tight junctions which, along with a lipid secretory material, make the epithelium a permeability barrier.
The vagina wall has no glands and so lubrication must come from the cervix and glands around the opening of the urethra.
The muscle coat in the vaginal wall is interlacing bundles of smooth muscle. There is a thin circumferential band of striated muscle around the ostium of the vagina.
The following figure is from your slide 84, showing a section of the vagina. Note the pale epithelia which are washed out probably because they contain glycogen and lipid.
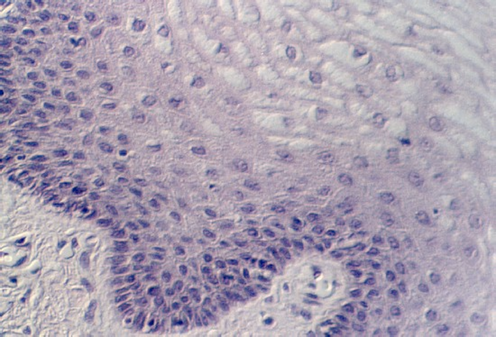
In the basal regions of the vagina epithelium, one may see lymphocytes and Langerhans cells. What important function (s) do the Langerhans cells play?
Gwen V. Childs, Ph.D., FAAA
Department of Neurobiology and Developmental Sciences
University of Arkansas for Medical Sciences
4301 W. Markham, Slot 510, Little Rock, AR 72205
For questions or concerns, send email to this address